
Spectrum physiotherapy centre pioneer in physiotherapy with more than 50 physiotherapists working under one roof. We are in Bangalore for since 1999 and the branches started expanding from 2006 and now extended into 16 locations . Started with the objective of providing ultimate foolproof evidence-based physiotherapy and rehabilitation services in client-centric western healthcare model in India. www.spectrumphysio.info
Dec 29, 2019
May 27, 2019
Sports Physiotherapist for knee pain
All injuries are not the same .
The bio mechanisms plays a major role
The bio mechanisms plays a major role
May 26, 2019
Best treatment for Disc Prolapse IVDP Lumbar Cervical disc problem
Long hours of sitting in front of the computer and holding the smart phone for more than 20 min continuously will lead to stress to the muscles ..
If this is ignored and persisted with nagging discomfort will lead to changing in Bio mechanical and pathomechanical alignments causing pain and degeneration .
For long standing chronic pain and Sciatica now the distraction force created in this De compression traction causes more healing rate to the disc .
With the decompression when the load bearing is monitored by the muscle length and strength by our team of physiotherapists has given very good recovery we can stay away from surgery for the certain type of Lumbar and Cervical disc issues .
http://www.spectrumphysio.info/blog/
If this is ignored and persisted with nagging discomfort will lead to changing in Bio mechanical and pathomechanical alignments causing pain and degeneration .
For long standing chronic pain and Sciatica now the distraction force created in this De compression traction causes more healing rate to the disc .
With the decompression when the load bearing is monitored by the muscle length and strength by our team of physiotherapists has given very good recovery we can stay away from surgery for the certain type of Lumbar and Cervical disc issues .
http://www.spectrumphysio.info/blog/
Apr 26, 2019
RETURN TO SPORT AFTER ACL INJURY
The anterior cruciate ligament (ACL) is one of four major knee ligaments used for stabilization of this joint. The ACL is the most significant ligament for rotational stability of the knee. Even after an ACL injury, the patient can still walk, climb stairs, and jog, but side-to-side activity is difficult and the knee will “give way.” When a tear to the ACL occurs, the patient often reports they hear a pop and feel a sharp shooting pain in the knee. The knee is often swollen after this type of injury, and it may become quite stiff.
Anterior cruciate ligament (ACL) reconstruction surgery is done to rebuild the ligament in the center of the knee with the patient’s own tissue (auto graft) or a donor’s tissue (allograft). The ACL keeps the tibia (shin bone) in place, and when it is torn, the knee will give way during exercise, walking, or physical activity. Here are some common myths about ACL reconstruction.
For athletes who wish to return to pivoting sports, the typical advice is an ACL reconstruction after 4–8 weeks when full range of motion is established and there is no joint swelling. The purpose of an ACL reconstruction is to give the athlete a mechanically stable knee and to reduce the risk of subsequent injury to the menisci and cartilage by reducing anteroposterior joint motion. A number of short-term studies have shown good to excellent knee function after reconstruction, whether hamstrings or patellar tendon grafts are used. The same studies also confirm that most patients (65–88%) are able to return to sport within the first year. Thus it is fair to state that surgery is effective in allowing injured athletes to resume their sports career.
Also, some athletes are able to return to high level pivoting sports without surgery. Among patients treated non-operatively, the return rate ranges from 19% to 82%. The athletes who successfully return to sport after non-operative treatment probably represent a selected group with functionally stable knees and a strong motivation to continue pivoting sport despite their injury.
If athletes can return to sport with or without ACL reconstruction, how long are they able to keep playing after the initial injury? Most studies deal with ACL reconstructed patients, and the results vary between studies with a range from 8% to 82%. However, it is not always clear whether the authors are reporting an initial return rate or the proportion still playing at the time of follow up.
Nevertheless, a few studies may be of particular interest, because they follow sports specific patient populations and report data on patients treated with and without surgery. Also, these studies mainly include elite athletes who can be assumed to be well motivated to continue their sports career. Thus the data may provide a realistic estimate of what to expect after returning to sport after injury. Myklebust et al9found in a 6–11 year follow up of ACL injured team handball players that 58% of the reconstructed players and 82% of the conservatively treated patients were able to return to their preinjury level.
In the 10–13 year follow up study with a mixed sport population, Fink et al13 found a 44% reduction in high risk sports participation in the surgically treated group compared with a 70% reduction among the conservatively treated. In the longest follow up to date, von Porat et.al., 14 showed that, after 14 years, 6% in the operatively treated group and 1% in the conservatively treated group were still playing soccer. However, from these studies it is not possible to determine whether the players retired because of the injury or whether the retirement rate was higher than can be expected. Clearly, athletes may quit for reasons unrelated to their knee injury.
In the only study in which the reduction in sport participation can be related to a control group, Roos et.al., 10 reported on elite soccer players three to seven years after the ACL injury. They found that 30% were active in soccer after three years compared with 80% in an uninjured control population. In addition, they showed that, after seven years, none of the injured elite players were active regardless of the type of treatment. It seems fair to conclude that, although the initial return rate is high, regardless of treatment, previously injured athletes retire at a higher rate than athletes without previous ACL injuries. The reason for this may be that many of the athletes who return to sport experience significant knee problems, such as instability, reduced range of motion, and/or pain.
RE-INJURY RATE AFTER SURGERY
One of the potential concerns with returning to sport is that the re-injury rate to the reconstructed ACL or to other structures (menisci, cartilage, or other ligaments) may be unacceptably high. Only few studies have examined re-injury risk, and they report a wide range of re-rupture rates ranging from 2.3% to 13%. The highest ACL re-rupture risk (13%) was found by Myklebust et al9 in their study of team handball players. However, one reasons for the high risk seen in this study may be that team handball in itself is a high-risk sport. Six of the 50 players who returned to team handball (9%) experienced an ACL tear in their contralateral, previously uninjured knee during the observation period. Drogset and Grontvedt reported a similar re-injury rate, who found that 12% of their patients suffered a re-injury during an eight year follow up period, all during pivoting sports.
However, these results, as well as studies reporting lower re-rupture rates, must be interpreted with caution. Firstly, the population at risk is not known, because it clearly depends on the proportion returning to sport and the number of years they continued to play. Secondly, bias must be considered when there is a significant loss to follow up as is evident in most of the studies. Thus, we do not know if there is an increased risk of re-injury to the reconstructed ACL compared with a healthy knee, nor do we know the rate of meniscus or cartilage injury associated with return to sport. Nevertheless, it is clear that nearly all of the re-ruptures reported in the papers shown in table 1 occurred while pivoting sports were being played.
“Returning to pivoting sport without a reconstruction results in considerable risk of injury to the menisci and cartilage”
Further damage to the knee with continued sports participation is of course also a concern in non-operatively treated patients. Myklebust et al9 showed that 22% of the non-operatively treated players who returned to sport underwent additional surgery for an injured meniscus compared with 12% in the operatively treated players. Returning to pivoting sport without a reconstruction results in considerable risk of injury to the menisci and cartilage.
ROLE OF PHYSIOTHERAPY IN CONSERVATIVE MANAGEMENT OF SLAP LESION
A SLAP tear or SLAP lesion is an injury to the glenoid labrum (fibrocartilaginous rim attached around the margin of the glenoid cavity). Tear of the superior labrum near to the origin of the long head of biceps means where this one of the tendon of biceps having attachment were first described among throwing athletes by Andrews in 1985. The label of ‘SLAP’, an abbreviation for superior labrum anterior and posterior, was coined by Snyder et al, who went on to create a classification system for these lesions.
An unstable shoulder joint can be the cause or the result of a labral tear. Injuries to the labrum are common and can cause a great deal of pain and may make it hard to move your arm. A labral tear can occur from a fall or from repetitive work activities or sports that require you to use your arms raised above your head (Overhead activity). Injuries to the superior labrum can be caused by acute trauma or by repetitive shoulder motion. The symptoms be like Deep aching pain, Popping, clicking, catching, locking or grinding in the shoulder, Inability to lie on the affected shoulder and pain while lifting the arm or object.
Role of physiotherapy
Physical therapy is the best non- operative treatment, Physical therapist is specialized to treat SLAP tear via conservative methods because SLAP lesion poses a significant challenge to the physical therapist due to its complex nature and wide variety of causative factors associated with these lesions. A thorough clinical evaluation and proper identification of the extent of labral injury is important in order to determine the treatment.
In SLAP lesion the Clinical examination revealed the Faulty posture of the shoulder, rounder shoulders, scapular dyskinesia (abnormal movement of shoulder blades during shoulder movement), Tenderness on the shoulder joint and upper arm, Trigger points over the scapular region, Decreased range of motion of shoulder, Weakness of scapular stabilization muscles. The exercise program is based on the extend of injury and the symptoms.
Marc – Andre Blanchette et, al study reported that conservative treatment to the slap lesion might provide an optimal recovery with a return to sports activities at the previous level or higher.
A recent study is showing the conservative, or non-operative, treatment of superior labral tears results in improvements in pain relief, shoulder function, and overall quality of life via the exercises i.e., scapular stability exercise, range of motion exercise, strengthening exercise etc,.
- Pain management is the first step of conservative management, the patient should abstain from aggravating activities in order to provide the pain relief. To control the pain can use heat or ice pack and electrical stimulation or TENS, trigger release therapy.
- Scapula stabilization exercises it specifically will help to improve the shoulder stability and mobility because stable shoulders are impossible without working this undertrained scapula musculatures i.e. rhomboids, serratus anterior, trapezius, levator scapulae, rotator cuff muscles. Shoulder joint does not act in isolation to create movement in arm. the muscles of shoulder and scapula act together to create all movement of the arm. Scapula stabilization exercise play important role to improve the overhead throwing motions, lifting weight overhead and restoring the proper position of the scapula and posture.
Shoulder shrugs- Shoulder bracing exercise
- Prone row
- Prone “T” scapula stabilization exercise
- Prone “Y’ scapula stabilization exercise
- Prone “I” scapula stabilization exercise




SCAPULA STABILIZATION EXERCISES
- Range of motion exercises which help to restore the normal
- shoulder movements. The restriction of range of motion is quite common in all shoulder pathology cases. In slap lesion the restriction of internal rotation, flexion and abduction is common. Range of motion exercise for shoulder is patient should move the shoulder actively through its full range (pain free).
- Active assisted range of motion exercise to shoulder
- Active range of motion exercise to shoulder
- Strengthening exercises should mainly focus on the muscle of rotator cuff (dynamic stabilizer). These four muscles surround the shoulder and help to keep shoulder in place while move the arm. Strengthening the muscles around the shoulder blade and arm also help to provide stability to shoulder after a slap tear.
- Isometric exercise to shoulder (flexors, extensors, internal rotators, external rotators, abductors).
- PNF Upper limb D1 and D2 patterns.
- Resistance band exercise to scapula, shoulder and elbow as follows:
Labels:
labrum tear,
shoulder pain,
spectrum physio
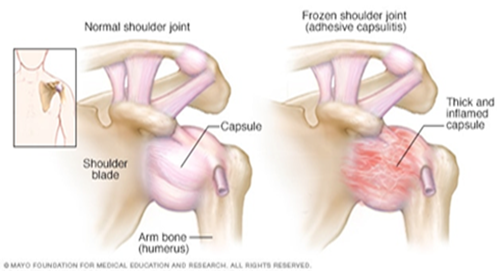
OVERVIEW OF FROZEN SHOULDER WITH CURRENT CONCEPTS OF PHYSIOTHERAPEUTIC MANAGEMENT
Frozen shoulder, also known as adhesive capsulitis, is defined as “a condition characterized by significant restriction of both active and passive shoulder motion that occurs in the absence of a known shoulder disorder.(1) Patients typically experience insidious shoulder stiffness, severe pain that usually worsens at night, and near-complete loss of passive and active external rotation of the shoulder.(2) It is likely that limitations in range of motion and the Shoulder pain associated with frozen shoulder are not only related to capsular and ligamentous tightness, but also Fascial restrictions, muscular tightness, and trigger points within the muscles.
Frozen shoulder can be classified as primary or secondary. Primary idiopathic frozen shoulder is often associated with other diseases and conditions, such as diabetes mellitus, and may be the first presentation of a diabetic patient.(3) Patients with systemic diseases such as thyroid diseases(4,5)and Parkinson’s disease(6)are at higher risk.
Secondary adhesive capsulitis can occur after shoulder injuries or immobilization (e.g. rotator cuff tendon tear, Subacromial impingement, biceps tenosynovitis and calcific tendonitis). These patients develop pain from the shoulder pathology, leading to reduced movement in that shoulder and thus developing frozen shoulder.
Frozen shoulder often progresses in three stages:
Stage 1: Freezing- In the "freezing" stage, you slowly have more and more pain. As the pain worsens, your shoulder loses range of motion. Freezing typically lasts from 6 weeks to 9 months.
Stage 2: Frozen- Painful symptoms may actually improve during this stage, but the stiffness remains. During the 4 to 6 months of the "frozen" stage, daily activities may be very difficult.(7,8)
Stage 3: Thawing- Shoulder motion slowly improves during the "thawing" stage as pain begins resolve. Return to normal or close to normal routine daily activities typically takes from 6 months to 2 years.(9,10,11)
Examination
Currently the diagnosis of primary adhesive capsulitis is based on the findings of the patient history and physical examination.(7)
1. Observation of posture and positioning
Eventually, patients with adhesive capsulitis develop adaptive postural deviations such as anterior shoulders or increased thoracic kyphosis as the function of the shoulder complex remains limited and painful, due to lack of capsular extensibility as well as a change in the central nervous system motor patterning due to maladaptive movement.
2. Movement pattern
In this condition the glenohumeral joint capsule will adhere to itself and not allow full motion. When this occurs there will be a very evident disturbance in the scapula-humeral rhythm. Any attempts at lifting hand on sideways (abduction) will usually require significant substitution and you will often see a motion like that pictured in the figure below, when an individual attempts abduction.
3. ROM screen: Active/passive/overpressure Range of motions.
Cervical, thoracic, shoulder ROMs with overpressure as well as rib mobility should be evaluated.
4. Resisted muscle tests -
Shoulder external rotation (ER) / Internal rotation (IR) / abduction (ABd) (seated) should be performed.
Patients with adhesive capsulitis present with weakness in shoulder ER, IR and ABd relative to the asymptomatic side.
5. Function related tests –
Common issues include :
-Unable to reach above shoulder height (Overhead activities).
-Unable to throw a ball.
-Unable to quickly reach for something.
-Unable to reach behind your back. E.g.: bra hooking or tucking shirt.
-Unable to reach out to your side and behind. E.g.: reach for seat belt.
-Unable to sleep on your affected side.
-Unable to reach above shoulder height (Overhead activities).
-Unable to throw a ball.
-Unable to quickly reach for something.
-Unable to reach behind your back. E.g.: bra hooking or tucking shirt.
-Unable to reach out to your side and behind. E.g.: reach for seat belt.
-Unable to sleep on your affected side.
PHYSICAL THERAPY INTERVENTIONS
Passive Motion:
Adhesive capsulitis involves fibrotic changes to the capsule-ligamentous structures, continuous passive motion or dynamic splinting are thought to help elongate collagen fibers. Recently, dynamic splinting was also used in patients with Stage 2 (“frozen stage”) adhesive capsulitis and the authors of the study, Gaspar and Willis, noted better outcomes when physical therapy was combined with the Dynasplint® protocol. (17)
Manual Techniques:
Joint mobilization is an effective intervention, several studies have demonstrated the effectiveness of joint mobilization in adhesive capsulitis patients.(12,18) In particular, posterior glide and anterior glide mobilization were determined to be more effective for improving external rotation range of motion. In addition, high-grade joint mobilization techniques are more effective than low-grade mobilization in improving glenohumeral mobility and reducing disability of patients with adhesive capsulitis.(19)
As discussed earlier, Myofascial trigger points, focal areas of increased tension within a muscle, may be present in the musculature around the shoulder complex in patients with adhesive capsulitis. The Spray and Stretch® technique for the Subscapularis and Latissimus dorsi muscle may be effective at reducing trigger point irritation, pain, and helping to gradually lengthen tight muscles.
Soft Tissue Mobilization:
Soft tissue mobilization and deep friction massage may benefit. Deep friction massage using the Cyriax method was shown to be superior to superficial heat and diathermy in treatment of patients with adhesive capsulitis. Recently, Instrument-Assisted Soft Tissue Mobilization (IASTM) as Graston Technique®, has become increasingly popular in physical therapy practice. IASTM reportedly provides strong afferent stimulation and reorganization of collagen, as well as in increase in microcirculation.
Therapeutic Exercise:
Pain is often most severe during the freezing phase and patients in this phase would benefit from learning pain-relieving techniques. These exercises include gentle shoulder mobilization exercises within the tolerated range (e.g. pendulum exercise, passive supine forward elevation, passive external rotation, and active assisted range of motion in extension, horizontal adduction, and internal rotation). Rotator cuff exercises, as well as posture exercises and exercises for the deltoid and chest also needed. A heat or ice pack can be applied as a modality to relieve pain before starting these exercises. The application of moist heat in conjunction with stretching has been shown to improve muscle extensibility.(19)
Once range of motion has progressed enough, strengthening to be an appropriate intervention. Strengthening exercises are added to maintain muscle strength. Isometric or static contractions are exercises that require no joint movement and can be done without worrying about increasing pain in the shoulder. Strengthening exercises can also progress from isometric or static contractions, Theraband exercises and Swiss ball and eventually to free weights or weight machines.

Modalities:
The rationale for using modalities in patients includes pain relief and affecting scar tissue (collagen). However, the use of modalities such as Ultra Sound Therapy, Iontophoresis, and Phonophoresis has not been proven to be beneficial in treatment of adhesive capsulitis.(12,13) Interestingly, Transcutaneous Electrical Nerve Stimulation (TENS) has been shown to significantly reducing pain. Recently, research also suggests that low-power laser therapy and deep heating through diathermy combined with stretching were shown to be more effective than superficial heating for treating frozen shoulder patients. (14,15,16)
In conclusion, this is a challenging condition for both the physical therapist and patient. It is important to make an accurate diagnosis and assessment in order to choose their best interventions. By understanding the published evidence related to the rehabilitation of patients with adhesive capsulitis, both therapists and patients will get benefit with an integrated, multi-faceted, evidence-based approach or interventions.
Subscribe to:
Posts (Atom)
